Mucormycosis: What You Should Know
Dr. Juni Banerjee, PhD, June 26, 2021
Mucormycosis is a fungal infection, also known as Black fungal disease. Its incidence seems to be increasing recently. This disease is rare, not contagious but is of great concern due to the association with high morbidity and mortality.
Rarity of the disease makes it hard to conduct large and randomized clinical trials, hence knowledge and data about its epidemiology, diagnosis and treatment mostly depends on the case-reports/series. As the clinical approach to diagnose mucormycosis lacks sensitivity and specificity, the treatment part also becomes late and challenging. This scientific article will address all the crucial queries related to the pathogenesis of mucormycosis.
What causes mucormycosis?
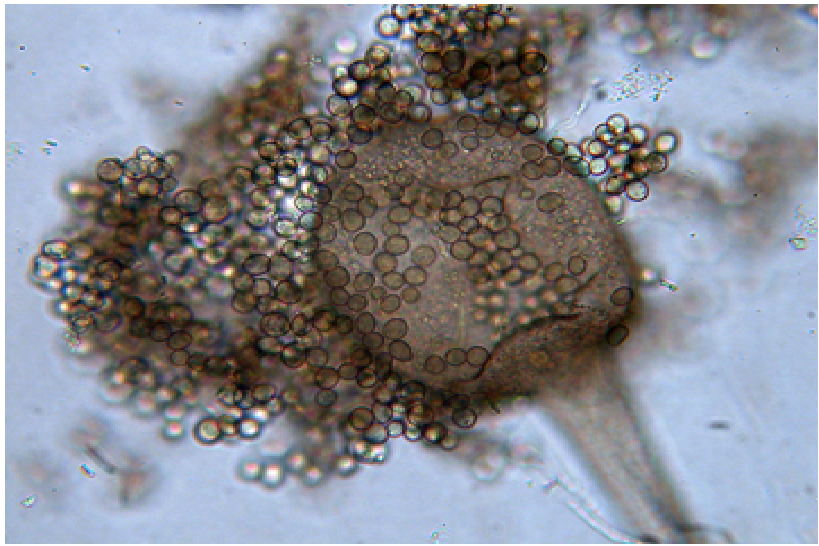
Mucormycosis is caused by a group of fungi called mucormycetes, that lives throughout our surrounding environment. Some of the examples of these fungi are: Rhizopus sp., Mucor sp., Rhizomucor sp., Syncephalastrum sp., Apophysomyces sp., and Lichtheimia sp. In India, Rhizopus sp. is the most common causative fungus for mucormycosis, however, Apophysomyces Elegans, A.Variabilis and Rhizopus Homothallicus are also being reported.
Who can get mucormycosis?
People who have either of the following health complications are more likely to get mucormycosis:
- Uncontrolled diabetes
- Cancer, Haematological malignancies and AIDS
- Undergone organ transplantation or stem-cell transplantation
- Under long-term corticosteroid medication or certain immunosuppressants
- Neutropenia (low number of white blood cells)
- Skin injuries due to surgery, scrape, wound or burns
- Infants with premature birth, underweight and immunity issues
- Even patients who have recently got rid of the coronavirus.
How does someone get mucormycosis?
Mucormycetes are present both in air and soil (mainly associated with decaying organic matter). Interestingly, these fungi are more common in soil than in air, and also in summer than in winter. It is impossible to avoid breathing air, getting exposed to soil, dust and the microscopic fungal spores.
Mucormycetes are harmful to people who have weakened immune system, or have other medical conditions as mentioned in the previous section. In such people a lung or sinus fungal infection might happen just by inhaling the fungal spores present in the air, or a skin fungal infection might happen following entry of the fungus through a skin cut, etc.

What are the types of mucormycosis?
- Pulmonary (lung) mucormycosis– Common in people with cancer or those who have undergone organ transplantation or stem cell transplantation.
- Rhinocerebral (sinus and brain) mucormycosis– Infection in the sinuses that can spread to the brain. It is common in severely diabetic and kidney-transplanted patients.
- Cutaneous (skin) mucormycosis– It is the most common form of mucormycosis in people who do not have weakened immune systems.
- Gastrointestinal (gut) mucormycosis– It is more common among young children, particularly premature and low birth-weight infants with low immunity.
- Disseminated mucormycosis– In this case the fungal infection spreads to other body parts (commonly the brain, but also heart, spleen etc) through the bloodstream. This is common in people who have had an organ transplant.
What are the symptoms of mucormycosis?
- Rhinocerebralmucormycosis– One-sided facial swelling, fever, headache, nasal or sinus congestion, black lesions on nasal bridge or upper inside of mouth.
- Pulmonary mucormycosis– Fever, cough, chest pain, shortness of breath.
- Cutaneous mucormycosis– blisters or ulcers, blackening of the infected area, pain, redness, swelling and warmness around a wound.
- Gastrointestinal mucormycosis– Abdominal pain, vomiting, gastrointestinal bleeding, and nausea.
- Disseminated mucormycosis– mostly the brain gets affected leading to mental status changes or even coma.
- Case-files have reported– excessive running nose, pain in the eyes, loss of vision as the other symptoms of this Black fungal disease.
How can one lower the risks of mucormycosis?
Importantly, no vaccine has been yet developed to prevent mucormycosis. Following are some of the recommended ways that might help to lower the risk of getting mucormycosis:
- Avoiding construction or excavation sites.
- Avoiding water-damaged buildings and flooded-water after hurricanes, floods etc.
- Wearing an N95 facial mask when outside.
- Wearing covered shoes, full-shirt and full-pants during outdoor activities e.g. visiting any wooded areas.
- Taking preventive measures while gardening- e.g., wearing appropriate gloves and masks when handling manure or moss.
- Frequent hand-wash with soap and water, if exposed to dust and soil.
- Cleaning skin-cut/burn/injuries with appropriate medicine.
- Taking prescribed antifungal medications (especially in case of patients who had an organ transplant or a stem cell transplant).
How does mucormycosis get diagnosed?
Following are helpful to diagnose the Black fungal disease:
- Symptoms, medical history, physical examinations are key to diagnose mucormycosis.
- Collection of fluid from respiratory system or a tissue biopsy (small sample of affected tissue) to be checked under a microscope (direct and histopathology) or by a fungal culture.
- Serological tests, Enzyme Linked Immunosorbent assays (ELISA), immunoblots etc.
- Computerized tomography (CT) scans of lungs, sinuses, or other infected body parts, often showing a reverse halo sign.
- Positron Emission Tomography (PET), matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF), Mass Spectrometry and Polymerase Chain Reaction (PCR).
- Radiological tests indicate- multiple (≥10) nodules and pleural effusion associated with pulmonary mucormycosis.
How can mucormycosis be treated?
Effective management of mucormycosis includes a multimodal approach:
- Discontinuation of underlying predisposing factors,
- Administration of optimum-dose antifungal medicines viz. amphotericin B, posaconazole, or isavuconazole. These medicines are given through a vein (amphotericin B, posaconazole, isavuconazole) or by mouth (posaconazole, isavuconazole).
- Surgical removal of infected tissues
- Applying adjunctive therapies
What is the link between mucormycosis and Covid-19?
Covid-19 pandemic continues to be a significant problem worldwide. Although, the Black fungal disease is being considered separate from Covid-19. Unfortunately, the widespread use of glucocorticoids for the treatment of Covid-19 is becoming a leading reason for secondary fungal as well as bacterial infections. Morecover, case studies are being reported for mucormycosis in case of patients who have just got rid of the coronavirus! Covid-19 patients, specially who have received steroids treatments are particularly at risk for mucormycosis because steroid drugs suppress the patient’s immune system. This is a point of concern as steroids should not be applied unless absolutely necessary. Scientists with in-vivo experiments have found that the inhaled mucor spores in healthy animals are quickly killed by white blood cells (WBC) of the immune system. In case the host’s immune response has been compromised, the body produces fewer WBCs. In this situation, the fungal spores germinate and grow rapidly as mycelium that branches out and enters the blood vessels and destroys them. Mucormycosis related illness can be fatal for acute, post-recovery or even asymptomatic covid-19 patients.
References:
- Garg D, Muthu V, Sehgal IS, et al. Coronavirus Disease (Covid-19) Associated Mucormycosis (CAM): Case Report and Systematic Review of Literature. Mycopathologia. 2021;186(2):289-298. doi:10.1007/s11046-021-00528-2
- Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum [published online ahead of print, 2021 Apr 8]. J Laryngol Otol. 2021;1-6. doi:10.1017/S0022215121000992
- Reid G, Lynch JP 3rd, Fishbein MC, Clark NM. Mucormycosis. Semin Respir Crit Care Med. 2020 Feb;41(1):99-114. doi: 10.1055/s-0039-3401992. Epub 2020 Jan 30. PMID: 32000287.
- Ibrahim AS, Spellberg B, Walsh TJ, Kontoyiannis DP. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54 Suppl 1(Suppl 1):S16-S22. doi:10.1093/cid/cir865
- Camara-Lemarroy CR, González-Moreno EI, Rodríguez-Gutiérrez R, et al. Clinical features and outcome of mucormycosis. Interdiscip Perspect Infect Dis. 2014;2014:562610. doi:10.1155/2014/562610
- Sen M, Lahane S, Lahane TP, Parekh R, Honavar SG. Mucor in a Viral Land: A Tale of Two Pathogens. Indian J Ophthalmol. 2021 Feb;69(2):244-252. doi: 10.4103/ijo.IJO_3774_20. PMID: 33463566; PMCID: PMC7933891.
- Riley TT, Muzny CA, Swiatlo E, Legendre DP. Breaking the Mold: A Review of Mucormycosis and Current Pharmacological Treatment Options. Ann Pharmacother. 2016 Sep;50(9):747-57. doi: 10.1177/1060028016655425. Epub 2016 Jun 15. PMID: 27307416.









