Formation of Blood Clots inside some Covid-19 patient’s Vital Organs: New Medical Findings
Dr. Shuvomoy Banerjee, PhD; from Neucrad Health desk, August 16, 2020
A new fact came into notice of scientists, due to the vast ongoing research on Covid-19. The interesting yet alarming finding is the presence of blood-clots in the blood vessels of the vital organs (like lungs, heart, kidneys) of severely affected Covid-19 patients!
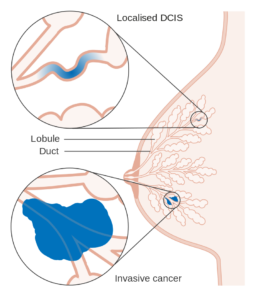
Dr. Amy Rapkiewicz, Chairman of the Department of Pathology at New York University Langone Medical Center, currently conducted Autopsy (subjected to permission) of the vital organs from the patients who died due to Covid-19. Surprisingly, their autopsy analysis indicated presence of blood clots in all types of blood vessels (large as well as small arteries and veins). Her research team observed the presence of ‘Megakaryocytes’ (a type of immune cell found only in the bone marrow and lungs) in patient’s heart, kidneys and liver!

According to researchers, megakaryocytes help in the formation of platelets or thrombocytes which play a crucial role in blood clotting. Henceforth, the scientists have reasoned that ‘cytokine storms’ due to Covid-19, not only causes severe inflammation but also formation of blood-clots inside the blood vessels associated with vital organs. “The Lancet Journal of E-Clinical Medicine” has accepted and published this work by Dr. Amy Rapkiewicz.
Blood Clotting and Covid-19: Relation
In medicine, the association of blood coagulation with infection is not new. But severe blood coagulation can cause “Disseminated Intravascular Coagulation (DIC)” resulting in blood-clots in patient’s bloodstream thus hindering the normal blood circulation. Usually, inflammation and blood clotting are like two-way traffic. In other words, inflammation induced blood-clots always try to reduce the inflammatory responses!
But in the case of Covid-19, the matter was not very clear. This is because the immune response is different and seen at different stages in the SARS-CoV-2 infected patients.
- In mildly-affected Covid-19 patients, the levels of pro-inflammatory cytokines (such as IL-6, IL-1 and TNF-alpha) in the blood initially increase and the symptoms of ‘cytokinemia’ appear, but within a few days it subsides.
- However, the patients with severe symptoms of Covid-19 demonstrate blood clots in the blood vessels of different organs in order to stop the transmission of the virus. During this time, the cytokine storm begins, which can cause failure of various organs and subsequently death of the patient.
In this context, more details came from the research team of Dr. Jeffrey Laurence (Professor of the Division of Hematology and Medical Oncology at Weill Cornell Medical Center) and his colleagues from the New York Presbyterian Medical Center. According to their study, many of the hospitalized Covid-19 patients showed blood-clots in the blood vessels of the lungs and brain. Even though physicians have been using blood thinner drugs (e.g. heparin) in large quantities, they are not getting effective responses.
Dr. Laurence and his researchers’ tireless efforts have discovered the reason behind such phenomenon. They found the crucial role of complement proteins (mainly C5) which is capable of destroying infected cells through a ‘cascade reaction’ in the immune system and also to cause blood clotting.
The researchers found that the molecular interaction of MASP-2 (complement protein) with spike protein of SARS-CoV-2 triggers the ‘complement cascade’ reaction in Covid-19. This reaction causes the blood to clot quickly. The details of these molecular events have been published in the research journal “Translational Research“.
At present, presence of Blood-clot in the Covid-19 patient’s vital organs needs special attention of the scientists and the physicians to conduct thorough research on it. Already, Dr. Jeffrey Laurence has begun investigating the effect of the drug ‘Argatroban’ (a new blood thinning agent) in blood coagulation due course of SARS-CoV-2 infection. In addition, researchers in the United States and Italy are planning for a clinical trial of the anti-complement drug “Eculizumab” to map and identify the critical points in complement cascade for influencing blood coagulation. People around the world are eagerly waiting to know the results and implications of their studies.



References:
- Rapkiewicz AV, Mai X, Carsons SE, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine. 2020;24:100434. Published 2020 Jun 25. doi:10.1016/j.eclinm.2020.100434
- Lax SF, Skok K, Zechner P, et al. Pulmonary Arterial Thrombosis in COVID-19 With Fatal Outcome: Results From a Prospective, Single-Center, Clinicopathologic Case Series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi:10.7326/M20-2566
- Buja LM, Wolf DA, Zhao B, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol. 2020;48:107233. doi:10.1016/j.carpath.2020.107233
- Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1-13. doi:10.1016/j.trsl.2020.04.007
- Noris M, Benigni A, Remuzzi G. Kidney Int. 2020 Aug; 98(2):314-322. Epub 2020 May 24.
- Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, et al. N Engl J Med. 2020 Jul 9; 383(2):120-128. Epub 2020 May 21.