Bengaluru doctors undertake a unique form of bone marrow transplant to save a 4-year-old boy

Neucrad Health News Desk February 3, 2020
In a heartening incident, doctors at the reputed Mazumdar Shaw Cancer Centre gifted a fresh lease of life to a 4-year-old boy Tanzanian boy through bloodless bone marrow transplant. The child belongs to Jehovah’s Witnesses faith practised at the East African country, where religious rules forbid blood transfusions as a treatment. Doctors always rise beyond the call of their professional duty when it comes to therapies of tiny souls. The treatment of Ittai James Moshi was no exception. Oncologists diagnosed abdominal cancer and suggested bone marrow transplant as the most preferred mode of treatment. However, since Ittai could not go ahead with standard marrow transfusion, doctors proposed unique bloodless transplantation for him.
How did doctors carry out Ittai James Moshi’s treatment?
Children suffering from certain forms of cancer like leukaemia and abdominal cancer go through bone marrow transplant for complete cure of the disease. However, Ittai’s faith did not allow him to follow this standard procedure as it involved blood transfusion. They wanted to explore other forms of cure in foreign countries to save the life of the child. In 2018, the boy along with his parents (who were IT professionals) flew down to Bengaluru for further treatment.
How is it possible to carry out bone marrow transplant without blood transfusion?
Ittai started with the treatment in September 2019 at the acclaimed Mazumdar Shaw Cancer Centre. A team of highly skilled and experienced medical staff continuously monitored his health condition round the clock. Dr Sunil Bhatt, director and clinical lead of paediatric oncology of the leading medical institute in Bangalore decided to harvest stem cells for the bone marrow transplant from Ittai’s own body. After retrieving the cells, they allowed it to regenerate in the laboratory. It took about three weeks for new marrow cells to develop from the extracted stem cells. After months of medical supervision, Itaai is recovering well from abdominal cancer. Through this revolutionary technique, oncologists could treat his abdominal malignancy without any blood transfusion. However, doctors also pointed out that this method of therapy involved more risk than the standard bone marrow transplant.

What is a Bone Marrow Transplantation?
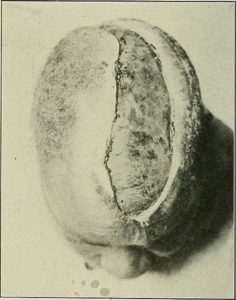
Bone marrow is a spongy and fatty tissue present within long bones and contains hematopoietic stem cells (HSC). They remain concerned with the production of red blood cells (RBC), white blood cells (WBC), and platelets. In some cases, marrow cells may get infected or damaged due to an underlying disease or chemotherapy. Doctors then recommend transfusion of blood stem cells, which ultimately reach the marrow and start regenerating new marrow cells. This procedure is known as bone marrow transplantation.
What are the different forms of Bone Marrow Transplantation?
There are two principal types of bone marrow transfusion- autologous transplant and allogeneic transplant.
Autologous Transplants

In this process, doctors harvest an individual’s own stem cells for regenerating new marrow cells. This type of treatment is only possible when the candidate has healthy bone marrow. It usually takes place before chemotherapy and radiotherapy. Though it is a complicated process, it reduces the risk of graft-versus-host disease (GVHD).
Allogeneic Transplants

In an allogenic transfusion, doctors retrieve healthy stem cells from a genetically matching donor. Usually, close relative acts as a donor for stem cells. However, if relatives are not available, then you can also check the donor register of stem cell banks for the marrow transfusion. Allogenic transplantation is a favoured procedure when the candidate does not have healthy bone marrow. However, it increases the risk of GVHD; the patient also receives immune-suppressant medications so that the immune cells do not attack the transfused stem cells.