SARS-CoV-2 and von Willebrand Factor: Complications in COVID-19
By Rahul Saha, PhD. August 4, 2020
The scientific community is gradually coming to the agreement on a hypothesis that the severe course of COVID-19 may be associated with the von Willebrand Factor (VWF), one of the main components of the blood coagulation system. As research suggests, the replication of the virus
stimulates the development of microdamage on the tunica intima layer of the capillaries which harbors endothelial cells. This consequently enhances the risk of thromboses.
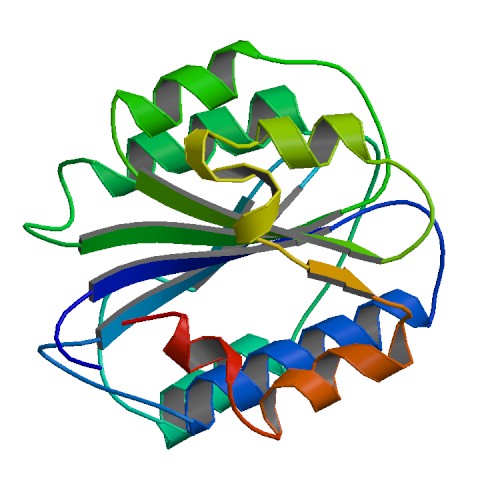
von Willebrand Factor is an adhesive and multimeric glycoprotein synthesized in the endothelial cells and megakaryocytes/thrombocytes. The VWF gene is transcribed into a 9 kb mRNA which is then translated into a protein of 2813 amino acids with an estimated molecular mass of 310,000
Da. Pre-pro-polypeptide VWF contains:
• 22 amino acids signal peptide
• 741 amino acids pro-polypeptide
• mature peptide.
The mature VWF subunit comprising of 2050 amino acids is formed after the cleavage of the 741 amino acids pro-polypeptide from its amino terminal end. The level and activity of VWF in the blood can differ among individuals. The homodimerization of pro-VWF subunits occurs in the
endoplasmic reticulum in a ‘tail-to-tail’ manner via formation of disulfide bonds between the Cterminal residues. The VWF dimers subsequently reach Golgi complex, where post translational modifications occur, like:
• proteolytic cleavage and removal of the large VWF peptide fragment
• addition of sulphate residues to N-linked oligosaccharides
• O-linked glycosylation.
In response to inflammation observed widely in case of COVID-19 patients, the level of VWF increases in circulation rapidly. Both the regulated and constitutive pathways are used for the secretion of VWF from endothelial cells. On the other hand, stimulation of megakaryocytes only leads to release of VWF via the constitutive pathway. There exists a litany of secretagogues and antagonists which can affect the pathways indulged in VWF secretion, expressed on both the endothelial cells and megakaryocytes. The secretagogues are categorized into two groups: (i)
cAMP elevating group and (ii) Ca2+ elevating group, whereas the VWF antagonists are hydrogen peroxide, nitric oxide and dopamine. The secretion of VWF into the plasma occurs in the form Ultra Large von Willebrand Factor (ULVWF) comprising of hundreds of VWF monomers. The ULVWF form keeps traversing in the bloodstream unless it gets divided into monomeric forms due to sheer stress forces emanating from molecular collisions with tunica intima layer of blood vessels. Three types of VWF exists in the human body:
• Extracellular matrix VWF/basement membrane VWF
• Cellular VWF
• Soluble plasma VWF
VWF has mainly three types of functions that mediates cellular homeostasis:
• Platelet adhesion
• Interaction with subendothelial matrix
• Carrier of Factor VIII
In case of an injury to a blood vessel membrane, the interaction of plasma VWF with the circulating thrombocytes occurs via two receptor membrane proteins: glycoprotein IIb-IIIa complex (GPIIbIIIa) and glycoprotein Ib (GPIb). The cross talk among thrombocytes and blood vessel wallthrombocyte adhesion is mediated by GPIIb-IIIa complex, whereas GPIb promotes blood vessel wall-thrombocyte adhesion.
VWF becomes extremely relevant in the above process as it’s the only ligand that is capable of binding to both GPIb and GPIIb-IIIa membrane receptors and thus, can facilitate platelet adhesion. VWF also mediates a pivotal role in commencing adhesion of platelets to the basement membrane/extracellular matrix (mainly collagen fibers) via perpetuation of binding between GPIb expressed on platelets and fibrin.
VWF also has been found to increase the half-life of Factor VIII, which is synthesized in liver and its deficiency leads to the manifestation of Haemophilia A. VWF can increase the stability of Factor VIII via the following mechanisms:
• downregulation of proteolytic degradation of Factor VIII via inhibiting its attachment to phospholipid-binding proteins
• prohibits the scavenger cell receptors from attaching to Factor VIII
• stabilizes the structural conformation of Factor VIII
• downregulation of the coagulation pathway on account of prevention of binding of activated factor IX to Factor VIII.
The lowest values of VWF are associated with the von Willebrand disease. It is a hereditary blood disease that is characterized by spontaneous bleeding. Additionally, it differs markedly among healthy people. VWF level is higher among African Americans compared to Europeans; in men than in women; in adults than in children; and in the elderly than in middle-aged people. Also, academic papers have described VWF and blood group relationship via GWAS studies, and found that level of VWF is lower among people with blood group O, and is higher among those with blood group A. The different amount and activity of VWF in people with different blood groups
have a very intriguing explanation, this protein is post translationally modified by oligosaccharide chains (glycosylation) of antigenic determinants present in the ABO blood group system. This consequently affects the stability and activity of VWF. Acute respiratory distress syndrome (ARDS), which often develops in patients with severe form of COVID-19, can also be associated with VWF. There are studies that use the paradigm of model animals and people, which suggest that higher the VWF level, higher is the probability of respiratory distress as increased VWF level can lead to thrombotic events and indirectly aggravate acute respiratory distress syndrome (ARDS).
The drugs chloroquine and hydroxychloroquine, that demonstrated efficacy in the early phase of clinical trials in COVID-19 patients do have the potential to regulate autophagy. Chloroquine is an inhibitor of autophagy, which inhibits the binding of autophagosomes to lysosomes by increasing the pH of lysosomes, resulting in the accumulation of degraded proteins in cells. Chloroquine has also been found to induce an autophagy independent severe disorganization of the Golgi and endo-lysosomal systems. Hence, delay in autophagy may contribute to the delayed release of various chemicals into the extracellular surroundings which can also include VWF and thus can attenuate thrombotic events in COVID-19 patients.
It has been shown in various clinical journals that VWF is upregulated in severely ill COVID-19 patients requiring mechanical ventilation and suffering from ARDS. VWF acts as a stabilizer of Factor VIII in the circulation. This stabilization occurs via the formation of a non-covalently bound VWF-Factor VIII complex that protects Factor VIII from degradation perpetrated by activated protein C, and localizes Factor VIII to sites of platelet plug and promotes formation of clot. As much as 20% of the total VWF is stored in the α granules of platelets. The symptoms perpetuated
by VWF level alteration in COVID-19 patients include coagulopathy, characterized by increased thrombotic and microvascular complications. Hence, increase in the level of VWF enhances the probability of thrombotic events. The scientific community has therefore set its sights firmly on
unraveling the regulation of VWF and its role in the prognosis of COVID-19 patients.
Let’s know about the author:


REFERENCES
- Mauro Panigada, Nicola Bottino, Paola Tagliabue, Giacomo Grasselli, Cristi Novembrino, Veena Chantarangkul et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020 Jul;18(7):1738-1742.
- Gui-Ping Luo, Bing Ni, Xia Yang and Yu-Zhang Wu. von Willebrand factor: more than a regulator of hemostasis and thrombosis. Acta Haematol. 2012;128(3):158-69.
- Flora Peyvandi, Isabella Garagiola and Luciano Baronciani. Role of von Willebrand factor in the haemostasis. Blood Transfus. 2011 May;9 Suppl 2(Suppl 2):s3-8.
- Mario Mauthe, Idil Orhon, Cecilia Rocchi, Xingdong Zhou, Morten Luhr, Kerst-Jan Hijlkema et al. Chloroquine inhibits autophagic flux by decreasing autophagosomelysosome fusion. Autophagy. 2018;14(8):1435-1455.
- Dan T Vogl, Edward A Stadtmauer, Kay-See Tan, Daniel F Heitjan, Lisa E Davis, Laura Pontiggia et al. Combined autophagy and proteasome inhibition: a phase 1 trial of hydroxychloroquine and bortezomib in patients with relapsed/refractory myeloma. Autophagy 2014 Aug;10(8):1380-90.
- David Ellinghaus, Frauke Degenhardt, Luis Bujanda, Maria Buti, Agustín Albillos, Pietro Invernizzi et al. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N Engl J Med. 2020 Jun 17.
- George Goshua, Alexander B Pine, Matthew L Meizlish, C-Hong Chang, Hanming Zhang, Parveen Bahel et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020 Aug;7(8):e575-e582.








