Role of monoclonal antibodies in cancer therapeutics

Dr. Juni Banerjee, Feb 5,2022 Neucard Health Desk http://www.fb.com/neucradhealthbengali
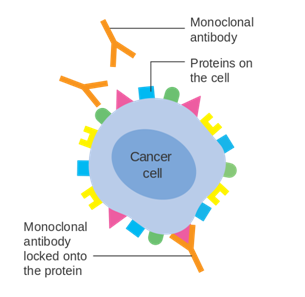
Monoclonal antibodies (mAbs) or mAb drugs have gained huge attention for their usage in cancer treatment. Monoclonal antibodies modulate human body’s immune system in a better and effective way for fighting against cancer cells and hence work as immunotherapy. The working mechanism of monoclonal antibodies can vary e.g., some mAbs can simply flag (mark) the cancer cells to make them easily recognized and eventually destroyed by the immune cells while some other mAbs can act as a delivery vehicle for chemotherapy or radiotherapy.
Which cancers are treatable with monoclonal antibody drugs?
Monoclonal antibody treatments have been developed and found more effective in the case of certain types of cancer cells like
- Brain cancer
- Head and neck cancers
- Breast cancer
- Lung cancer
- Stomach cancer
- Chronic Lymphocytic Leukemia (CLL)
- Hodgkin’s lymphoma
- Non-Hodgkin’s lymphoma
- Melanoma
- Prostate cancer
- Colorectal cancer
What are mAbs and what’s their origin?
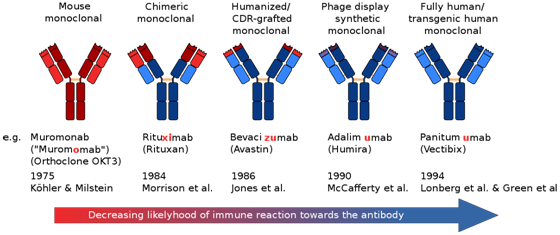
Monoclonal antibodies are human-designed proteins that can act just like the antibodies in the immune system. According to what they are made up of, mAbs can be either:
- Human mAbs – they are developed from human proteins and the names of human mAb treatment end in -umab.
- Murine mAbs – they are made from mouse proteins and the names of the murine mAb treatment end in -omab.
- Chimeric mAbs – they are developed in combination from both mouse as well as human proteins. The names of the chimeric mAb treatment end in -ximab.
- Humanized mAbs – theyare specially made from small parts of mouse proteins attached to human proteins. The names of the treatment with humanized mAb end in -zumab.
Major types of mAbs used in cancer treatment
- Naked mAbs- they are the most common type of cancer-treating mAbs. Naked mAbs can work in the following mentioned ways:
- by flagging the cancer cells and acting as a marker for the body’s immune cells, e.g., alemtuzumab (Campath®) that can bind to CD52 antigen of the chronic lymphocytic leukemia (CLL) cells
- by attaching and blocking cancer cell growth and metastasis promoting antigens on the cancer cells or neighbouring cells, e.g., trastuzumab (Herceptin) bind to the HER2 protein (highly present on breast cancer cell surface) and prevent its activation to stop breast cancer cell growth.
- Conjugated mAbs- Conjugated mAbs (also called tagged, labeled, or loaded antibodies) are those mAbs that are combined with a chemotherapy drug or a radioactive particle. They can act as a delivering vehicle for radiotherapy or chemotherapy directly to the cancer cells. Ibritumomab tiuxetan (Zevalin) is an e.g., of a radiolabeled mAb against the antigen CD20 (found on B lymphocytes) which is made of both a mAb drug (rituximab) and a radioactive substance (Yttrium-90). Example of a chemolabeled antibody includes Brentuximab vedotin (Adcetris), an antibody that targets the CD30 antigen (found on lymphocytes) and is attached to a powerful chemo drug called MMAE.
- Bispecific mAbs- These drugs are made up of parts of 2 different mAbs with an ability to attach with two different proteins at the same time. Blinatumomab (Blincyto) which is used to treat certain types of leukemia is an example of bispecific mAb, where one part attaches to the CD19 protein, (present on some leukemia and lymphoma cells) and another part can attach to CD3 protein (present on T lymphocytes), causing the immune system to attack the cancer cells effectively.
How do monoclonal antibody drugs work against cancer?
The working of mAb treatment depends on the type and stage of cancer and also on the nature of any ongoing treatment for the cancer patient. Generally, mAbs are administered intravenously. Moreover, some mAb drugs are also used in combination with other treatments (e.g., chemotherapy). Follwing are the ways in which mAbs works:
- By marking cancer cells- Cancer cells that are coated with certain type of mAb get easily detected and destroyed by the immune cells.
- By blocking cancer cell growth: Some mAb drugs work by blocking proteins required for tumor cell’s growth and survival.
- By triggering cancer cell-membrane destruction: Some mAbs can trigger an immune system response to destroy cancer cell’s outer membrane and consequently kill them.
- By preventing growth of blood vessels: Certain mAb drugs can prevent the growth and development of new blood vessels thus, hindering the survival and growth of the cancerous tumor.
- By acting as a delivery vehicle for radiotherapy: some mAbs are engineered as a delivery vehicle for radiotherapy. This method is also called radioimmunotherapy where the mAb is attached to a small and specific radioactive particle which can be directly transported to the cancer cells. This minimizes the side-effects of radiation on the normal cells.
- By acting as a delivery vehicle for chemotherapy: certain mAbs are designed for getting attached to powerful chemotherapeutic drugs in order to directly delivering powerful chemotherapy to cancer cells and not to healthy ones.
- By binding to both cancer and immune cells- Some mAb drugs are combination of two monoclonal antibodies in which one can attach to cancer cell and the other to specific immune cells. This way the mAb boosts the immune system to effectively target the cancer cells.
What are the side effects of mAb drugs?
Depending on a) individual health, b) type and stage of cancer, and c) the type and dose of mAb drug for the cancer treatment, there can be following types of side-effects:
- needle site reactions or skin reaction demonstrating pain, swelling, soreness, redness, itchiness, hives, rash are some common side-effects.
- Flu-like symptoms such as chills, fatigue, fever, muscle aches and pains, nausea, vomiting, diarrhea can also be seen commonly.
- Mild allergies.
- Skin, mouth, cheek and gum sores are common too.
- Severe side-effects are rare and may involve a) infusion reactions (severe allergic reactions during or soon after the administration of the mAb drugs, b) heart related problems (high blood pressure, congestive heart failure or heart attack), c) lung problems (inflammatory lung disease), d) capillary leak syndrome (tiny blood vessels oozes fluid and proteins into surrounding tissues) resulting in fatally low blood pressure as well as multiple organ failure, e) cytokine release syndrome (sudden increase in cytokine levels) leading to rapid heartbeat, trouble breathing etc f) severely and persistently low blood cell counts g) internal bleeding h)
References:
- Scott AM, Allison JP, Wolchok JD. Monoclonal antibodies in cancer therapy. Cancer Immun. 2012;12:14.
- Shuptrine CW, Surana R, Weiner LM. Monoclonal antibodies for the treatment of cancer. Semin Cancer Biol. 2012;22(1):3-13. doi:10.1016/j.semcancer.2011.12.009
- Cruz E, Kayser V. Monoclonal antibody therapy of solid tumors: clinical limitations and novel strategies to enhance treatment efficacy. Biologics. 2019;13:33-51. Published 2019 May 1. doi:10.2147/BTT.S166310
- Weiner GJ. Building better monoclonal antibody-based therapeutics. Nat Rev Cancer. 2015;15(6):361-370. doi:10.1038/nrc3930
- Chames P, Van Regenmortel M, Weiss E, Baty D. Therapeutic antibodies: successes, limitations and hopes for the future. Br J Pharmacol. 2009;157(2):220-233. doi:10.1111/j.1476-5381.2009.00190.x