Kidney transplantation from a HIV positive donor (US) and a brain death donor (India) – what do we learn?
By Neucrad Health news desk April 18, 2019
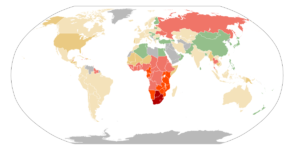
In a rare and unprecedented event an Atlanta based HIV-positive women, served as a kidney donor for another HIV-positive patient at Johns Hopkins Medicine in Baltimore. Both the donor and the recipient (wants to remain anonymous) are doing fine after the organ transplant. Dr. Dorry Segev, surgeon and professor at Johns Hopkins University School of Medicine had conducted surgery. According to him, the historic kidney transplantation is a rare achievement in HIV medical care.
A 36-year-old public health consultant who acquired HIV infection by receiving HIV-positive blood transfusion when she was merely six-year-old baby in 1983. In those days blood banks did not have the practice of routinely checking blood samples for different groups of viruses. However, the infection did not demoralise her, and she always has a desire of helping others with similar conditions.
What was it considered risky for HIV-Positive Individuals to act as an Organ Donor?
HIV attacks the immune system of infected patients. Earlier it was considered too risky for an HIV positive person to donate his kidney, as the HIV infection and the prescribed medications increase the chance of renal diseases. Urologists perceived that it would be dangerous for someone with this infection to live with a single kidney. However, this misconception has been abolished now with the revolutionary surgery conducted at Johns Hopkins Medicine in Baltimore.
How did the scenario involving HIV-Positive Organ Donors change?
A study on 42000 people in 2017 by the research scholars of Hopkins University proved that the chances of HIV-positive patients of developing kidney disease were not too high as compared to HIV-negative individuals. Moreover, the advanced antiretroviral medicines are safe for a kidney, so there are fewer chances of any complications after the organ donation. When the donor learnt that approximately 113000 candidates in the United States are on the organ transplant waiting list and one of her HIV-positive Facebook friends required kidney for survival, she decided on kidney donation.
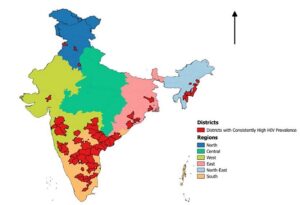
Organ Donations from a 13-Year-Old Brain Dead Girl in West Bengal, India
In a similar event in West Bengal of India, a thirteen-year-old brain dead girl was able to save three lives by donating her liver, kidney, and cornea to expecting candidates. The rare incident took place in November 2018 when doctors from Seth Sukhlal Karnani Memorial (SSKM) hospital in Kolkata travelled all the way to Durgapur to retrieve these organs. The medical team transported these organs to 170 kilometres away in Kolkata in just two hours through a green corridor with the help of police. The family took this step after they realised their daughter would remain alive through other people. Though the Human Organ Transplant Act 1994 has approved cadaveric transplant, in India there is a long list of about 210000 patients awaiting organ transplantation. These sort of initiatives by families will help to save many lives in future.
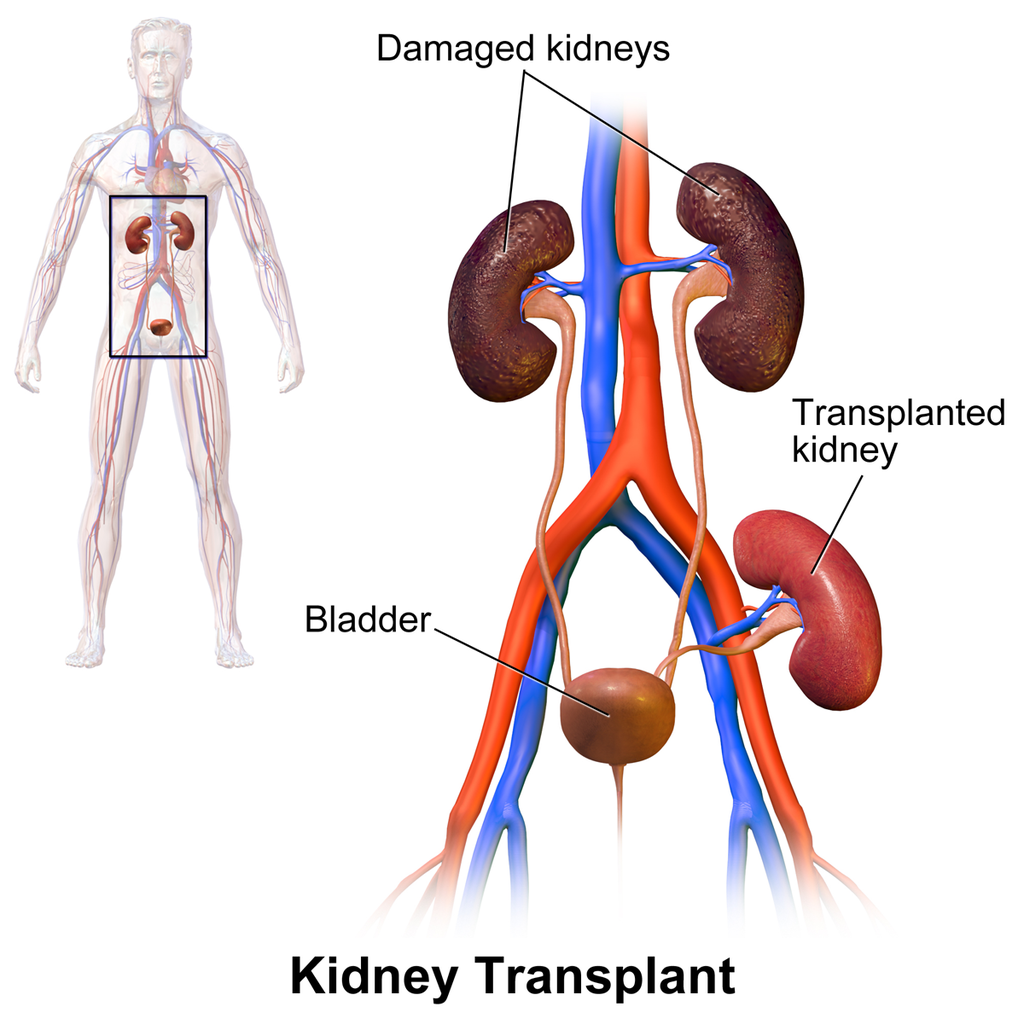
Matching Factors for Organ Donation
For successful organ transplantation, medical team carry out a thorough analysis of matching factors of the donor and recipient. It is primarily done so that the transplanted organ remain tolerated by the blood and tissues of recipient candidate indefinitely. For most organ transplantation like kidney, cornea, lungs, heart, and liver doctors match the blood groups, body size, consideration of Percent Reactive Antibody (PRA), and serum crossmatch. In the United States, the computer system of Organ Procurement and Transplantation Network (OPTN) scans these matching factors for donor and recipient. It also takes the severity of the recipient’s medical condition, and the distance between the donors and the recipient’s hospital into consideration before allocating the match.
Image credit: Kidney Transplant By BruceBlaus – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=44925836